Basilar membrane pathologies and hearing disorders can irrevocably alter your world, often leading to permanent hearing loss. Imagine a tiny, delicate structure deep within your inner ear, vibrating in response to every sound, from a whispered secret to a symphony orchestra. This microscopic marvel is the basilar membrane, and when it's compromised, the rich tapestry of sound begins to unravel. Understanding this vital component of our auditory system isn't just for audiologists; it's crucial for anyone seeking to protect their hearing and grasp the complexities of hearing impairment.
In this guide, we’ll dive deep into the world of the basilar membrane – what it is, how it works, and critically, what happens when it's damaged. We'll explore the causes, the consequences, and the proactive steps you can take to safeguard your irreplaceable sense of hearing.
At a Glance: Understanding Your Basilar Membrane and Hearing Loss
- Your Inner Ear's Maestro: The basilar membrane is a flexible, critical structure in the cochlea that converts sound vibrations into electrical signals your brain understands.
- The "Place Code": Different parts of the membrane respond to different sound frequencies (pitches) – the base for high notes, the apex for low notes.
- Fragile Sensors: It supports delicate hair cells, which are the true sensory receptors for hearing.
- Permanent Damage: Unlike many other cells in your body, human hair cells on the basilar membrane do not regenerate once damaged.
- Common Culprits: Loud noise, aging, and certain medications are leading causes of basilar membrane damage.
- Sensorineural Hearing Loss: Damage to the basilar membrane and its hair cells typically results in this type of permanent hearing loss.
- Hope for Management: While damage is often permanent, hearing aids, cochlear implants, and auditory rehabilitation can significantly improve quality of life.
The Inner Ear's Unsung Hero: What is the Basilar Membrane?
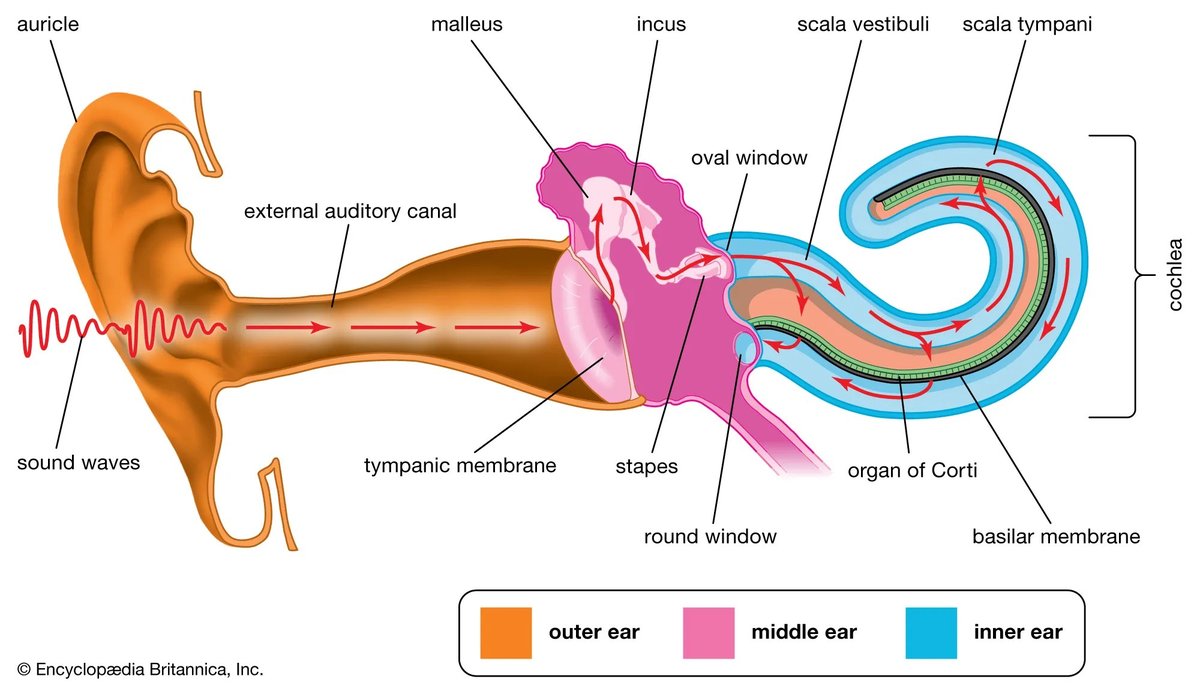
Deep within the temporal bone of your skull lies your inner ear, a complex labyrinth of fluid-filled canals. The star of the show for hearing is the cochlea, a tiny, snail-shaped structure that houses the basilar membrane. Think of the cochlea as a miniature grand piano, and the basilar membrane as the soundboard, meticulously tuned to capture every note.
This membrane acts as a crucial partition, separating two fluid-filled chambers within the cochlea: the scala media and the scala tympani. It stretches horizontally from a bony shelf called the spiral lamina to the outer wall of the cochlea, anchored by the spiral ligament. But it's no uniform strip; its physical characteristics are remarkably varied along its length, a design essential for its function.
At the base (the end closest to your middle ear's oval window), the basilar membrane is quite narrow, only about 0.08 to 0.16 millimeters wide, and relatively stiff. As it winds its way towards the apex (the center of the snail's curl), it gradually widens to 0.42 to 0.65 millimeters and becomes significantly more flexible. This ingenious gradient in stiffness and width is what allows different parts of the membrane to resonate, or vibrate, uniquely to different sound frequencies.
Crucially, the basilar membrane is also the foundation for the organ of Corti, an intricate structure often called the "true organ of hearing." This organ contains thousands of tiny, delicate sensory hair cells – the actual transducers that convert mechanical vibrations into electrical signals. View the basilar membrane schematic to truly appreciate this amazing architecture.
How We Hear: The Basilar Membrane's Role in Sound Processing
The journey from a sound wave in the air to a meaningful interpretation in your brain is nothing short of miraculous, and the basilar membrane is a key orchestrator of this process. It performs a sophisticated frequency analysis, allowing you to distinguish between a high-pitched violin and a deep bass drum.
Here's how it works:
- Sound Enters the Cochlea: When sound waves reach your inner ear, they cause the fluid within the cochlea to move. This fluid motion, in turn, makes the basilar membrane vibrate.
- The "Place Code" (Tonotopy): As these vibrations travel along the membrane, a specific point experiences maximum displacement, or the strongest vibration. The location of this maximum displacement depends entirely on the sound's frequency. This spatial mapping of frequency is known as tonotopy or a "place code."
- High-frequency sounds (like a child's scream or a high-pitched bell) cause the narrower, stiffer base of the membrane to vibrate most intensely.
- Low-frequency sounds (like a rumble of thunder or a cello's deep note) cause the wider, more flexible apex of the membrane to experience the greatest vibration.
- Hair Cell Activation: The membrane's movement causes the hair cells within the organ of Corti to shift. The microscopic "hairs" (cilia) on these cells bend against an overlying structure called the tectorial membrane.
- Electrical Signal Generation: This bending action is the critical step. It opens tiny channels in the hair cells, triggering a cascade of electrochemical events that generate electrical signals.
- Transmission to the Brain: These electrical signals are then transmitted to the auditory nerve and subsequently to your brain's auditory cortex, where they are interpreted as specific sounds – speech, music, or environmental noises.
This intricate process allows your auditory system to distinguish between an enormous range of frequencies, perceive complex sounds, and ultimately understand speech, even in challenging acoustic environments.
When Things Go Wrong: Basilar Membrane Pathologies and Their Impact
The exquisite precision of the basilar membrane makes it incredibly vulnerable. Any disruption to its structure or the delicate hair cells it supports can lead to significant hearing impairment. When we talk about basilar membrane pathologies, we're primarily referring to damage that prevents it from vibrating correctly or from effectively transmitting signals to the brain.
The most common outcome of such damage is sensorineural hearing loss (SNHL). This type of hearing loss occurs when there's damage to the inner ear (including the basilar membrane and hair cells) or the auditory nerve pathways to the brain. Unlike conductive hearing loss, which involves issues in the outer or middle ear, SNHL is typically permanent.
A critical, and often disheartening, fact is that human hair cells – those tiny sensors on the basilar membrane – do not regenerate once they are damaged or destroyed. This means that any hearing loss due to hair cell damage is, for now, irreversible. When these cells are lost, the specific frequencies they were tuned to can no longer be processed effectively, creating "gaps" in your hearing.
This damage often manifests as difficulty understanding speech, particularly in noisy environments. You might hear sounds, but your brain struggles to convert them into meaningful words. It's like trying to listen to a conversation through a crackling radio – the sound is there, but the clarity is lost.
Silent Assault: Common Causes of Basilar Membrane Damage
While the basilar membrane and its hair cells are incredibly resilient in some ways, they are also highly susceptible to certain environmental and biological factors. Understanding these common culprits is the first step toward prevention.
Acoustic Trauma: The Loud Noise Threat
One of the most pervasive threats to your basilar membrane is prolonged exposure to loud noise, often referred to as acoustic trauma or noise-induced hearing loss. Sounds exceeding 85 decibels (dB) can permanently harm these delicate structures. To put that in perspective:
- 85 dB: Heavy city traffic, a noisy restaurant
- 100 dB: Motorcycle, factory noise, power tools
- 110 dB: Live rock concert, car horn
- 120 dB: Ambulance siren
- 140 dB: Firecracker, gunshot, jet engine take-off
The damage isn't always immediate; it often accumulates over time. Think of it like bending a paperclip repeatedly – eventually, it breaks. Similarly, intense vibrations from loud noise can physically damage the hair cells, causing their cilia to break or the cells themselves to die. The high-frequency hair cells at the base of the cochlea are often the first to suffer damage from noise exposure, leading to difficulty hearing high-pitched sounds.
The March of Time: Presbycusis and High-Frequency Loss
Aging, or presbycusis, is another leading cause of basilar membrane-related hearing loss. As we get older, our bodies naturally undergo changes, and the inner ear is no exception. Age-related hearing loss frequently involves the gradual loss of sensory hair cells, particularly those located in the basal turn of the cochlea, which are responsible for processing high-frequency sounds.
This is why many older adults find it challenging to hear high-pitched voices, children's voices, or to follow conversations in crowded rooms where background noise masks higher frequencies. Presbycusis often progresses slowly and symmetrically, affecting both ears similarly, and is a result of a lifetime of wear and tear, combined with cellular degeneration.
Ototoxic Medications: Unintended Consequences
Unfortunately, some essential medications, while life-saving or disease-modifying, can have toxic side effects on the inner ear. These are known as ototoxic drugs. They can damage various structures within the cochlea, including the hair cells on the basilar membrane, leading to permanent hearing loss or tinnitus (ringing in the ears).
Key examples include:
- Aminoglycoside antibiotics: Drugs like gentamicin, tobramycin, and amikacin are potent antibiotics used to treat serious bacterial infections. However, they can accumulate in the inner ear fluid and directly damage hair cells.
- Chemotherapy agents: Cisplatin, a widely used chemotherapy drug for various cancers, is highly effective but also notoriously ototoxic. It can cause irreversible damage to the cochlear structures, leading to significant hearing loss in cancer patients.
- Loop diuretics: While less common for permanent damage, some high-dose loop diuretics can cause temporary hearing loss by altering the fluid balance in the inner ear.
It's crucial to discuss the potential ototoxic effects of any prescribed medication with your doctor, especially if you have existing hearing issues or risk factors.
Spotting the Signs: Recognizing Basilar Membrane-Related Hearing Loss
Recognizing the signs of hearing loss related to basilar membrane damage is crucial for early intervention and management. Because hair cell damage is permanent, timely diagnosis helps prevent further deterioration and allows for effective rehabilitation strategies.
Common symptoms you might experience include:
- Difficulty understanding speech: Especially problematic in noisy environments, over the phone, or when multiple people are talking. You might hear the words, but they sound muffled or unclear.
- High-frequency hearing loss: Struggling to hear sounds like birds chirping, doorbells, microwave beeps, or certain consonants (s, f, th, h).
- Tinnitus: A persistent ringing, buzzing, hissing, or roaring sound in one or both ears. Tinnitus is a common companion to inner ear damage.
- Muffled or distorted sound: Sounds may not seem as clear or distinct as they once did.
- Needing to turn up the volume: Frequently increasing the volume on the TV, radio, or phone.
If you notice any of these symptoms, it's wise to consult a hearing healthcare professional.
Diagnostic Methods
Diagnosing basilar membrane-related hearing loss typically involves:
- Audiogram: This is a standard hearing test that measures your hearing sensitivity across different frequencies. It can pinpoint specific frequency losses indicative of inner ear damage.
- Otoacoustic Emissions (OAEs): These tests measure faint sounds produced by healthy outer hair cells in the cochlea. Absent or reduced OAEs can indicate damage to these cells.
- Auditory Brainstem Response (ABR): This test measures how the auditory nerve and brainstem respond to sound, helping to assess the integrity of the auditory pathway beyond the cochlea.
These diagnostic tools help determine the type, degree, and configuration of your hearing loss, guiding treatment decisions.
Navigating the Future: Management and Treatment Options
While current medical science cannot regenerate damaged hair cells or fully repair a compromised basilar membrane, significant advancements in technology and rehabilitation offer effective ways to manage the impact of these pathologies and improve quality of life.
Current Approaches to Hearing Loss Management
- Hearing Aids: For many individuals with mild to severe sensorineural hearing loss, hearing aids are the first line of defense. These devices amplify sounds, making them louder and clearer, thus utilizing any remaining healthy hair cells and residual hearing capacity. Modern hearing aids are highly sophisticated, featuring advanced digital processing, noise reduction, and directional microphones to help you hear better in various environments.
- Cochlear Implants: For those with severe to profound hearing loss where hearing aids offer limited benefit, cochlear implants can be life-changing. These devices bypass the damaged hair cells of the basilar membrane entirely. An external processor captures sound and transmits it to an internal implant, which then directly stimulates the auditory nerve. This creates a sense of hearing that, while different from natural hearing, can allow individuals to perceive speech and environmental sounds.
- Auditory Rehabilitation and Aural Training: Beyond devices, rehabilitation plays a crucial role. This includes speech reading (lip-reading), auditory training exercises to help the brain adapt to amplified or artificially generated sounds, and communication strategies to navigate challenging listening situations. The goal is to maximize your remaining hearing abilities and improve your ability to communicate effectively.
- Assistive Listening Devices (ALDs): These devices, such as personal FM systems, amplified telephones, and TV listeners, can further enhance communication in specific situations by reducing background noise and improving the signal-to-noise ratio.
Preventative Measures: Taking Control
Since basilar membrane damage is largely irreversible, prevention is paramount.
- Protect Your Ears from Loud Noise: This is perhaps the most critical step.
- Wear earplugs or earmuffs when exposed to loud noises (concerts, sporting events, power tools, lawn mowers, shooting ranges).
- Limit your time in noisy environments.
- Turn down the volume on personal listening devices. The "60/60 rule" (listening at 60% volume for no more than 60 minutes at a time) is a good guideline.
- Be Aware of Ototoxic Drugs: Always discuss the potential side effects of medications with your doctor or pharmacist. If you must take an ototoxic drug, your doctor may monitor your hearing during treatment.
- Manage Underlying Health Conditions: Conditions like diabetes, high blood pressure, and cardiovascular disease can affect blood flow to the inner ear, potentially contributing to hearing loss. Managing these conditions can support overall ear health.
- Regular Hearing Check-ups: Especially as you age, periodic hearing tests can detect subtle changes early, allowing for timely intervention and counseling.
Your Questions Answered: Basilar Membrane & Hearing Health FAQs
Can the basilar membrane heal itself?
Unfortunately, the human basilar membrane and, more specifically, the hair cells it supports, do not regenerate or heal themselves once damaged or destroyed. While some research explores gene therapy and stem cell treatments for hair cell regeneration, these are still in experimental stages and not available clinically.
Is damage to the basilar membrane always permanent?
Damage to the hair cells on the basilar membrane typically results in permanent sensorineural hearing loss. However, some very mild forms of noise-induced trauma might cause temporary threshold shifts, where hearing recovers after a period away from noise. For the most part, once hair cells are gone, the hearing loss is permanent.
How can I protect my basilar membrane?
The best way to protect your basilar membrane is to avoid excessive noise exposure by wearing hearing protection (earplugs, earmuffs) in loud environments, limit the volume and duration of personal audio device use, and be mindful of ototoxic medications. Maintaining overall health through diet and exercise also supports inner ear health.
What's the difference between conductive and sensorineural hearing loss?
Conductive hearing loss occurs when there's a problem with sound transmission through the outer or middle ear (e.g., earwax blockage, fluid in the middle ear, eardrum perforation). This type of hearing loss is often temporary and treatable. Sensorineural hearing loss (SNHL), on the other hand, results from damage to the inner ear (including the basilar membrane and its hair cells) or the auditory nerve. SNHL is typically permanent and often involves issues with clarity and understanding, not just loudness.
Taking Action: Safeguarding Your Hearing for a Lifetime
Your hearing is a precious gift, allowing you to connect with the world, enjoy music, and communicate with loved ones. The basilar membrane, though tiny, plays an outsized role in this ability. Understanding its function and vulnerabilities empowers you to make informed decisions that can preserve your hearing for years to come.
Don't wait until sounds begin to fade or voices become muffled. Be proactive: protect your ears from loud noise, be aware of the medications you take, and seek professional help at the first sign of any hearing change. Early detection and intervention, combined with the incredible advancements in hearing technology, can significantly mitigate the impact of basilar membrane pathologies, ensuring you continue to experience the richness of the auditory world. Your future self will thank you.